Physical Therapy Guide to Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease, or COPD, is a lung condition that involves prolonged respiratory symptoms. These symptoms include shortness of breath, cough, and sputum (phlegm) production that can limit a person’s activity. With COPD, abnormalities in the airways used for breathing lead to airflow problems. Smoking, indoor and outdoor air pollution, and abnormal lung development are the primary causes of the condition. Genetic factors also may cause abnormal lung function, leading to COPD.
COPD is the third leading cause of death worldwide (3.23 million deaths in 2019). Nearly 90% of COPD deaths in those under 70 years old occur in low- and middle-income countries. It is the seventh leading cause of poor health worldwide. Tobacco smoking accounts for over 70% of COPD cases in high-income countries. It accounts for up to 40% in low- and middle-income countries, where air pollution is also a major risk factor.
Physical therapists help people with COPD improve their symptoms and restore strength in their breathing muscles. They help them build breathing efficiency, increase activity tolerance, and reduce fatigue through guided exercise programs.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To locate a physical therapist in your area, visit Find a PT.
What Is Chronic Obstructive Pulmonary Disease?
With COPD, the airways in your lungs lose their normal shape and elasticity. They also can become inflamed. This results in the airways being less efficient at moving air in and out of your lungs. Primary risk factors for developing COPD include:
- Smoking.
- Inhaling toxic substances.
- Indoor and outdoor air pollution.
- Genetic factors and environmental interactions.
- Abnormal lung development during prenatal or early childhood stages of life.
The most common types of COPD are:
Chronic bronchitis. A chronic inflammation of the medium-sized airways, or bronchi, in the lungs. Chronic bronchitis causes a cough that persists and produces sputum and mucus lasting at least three months per year, two years in a row.
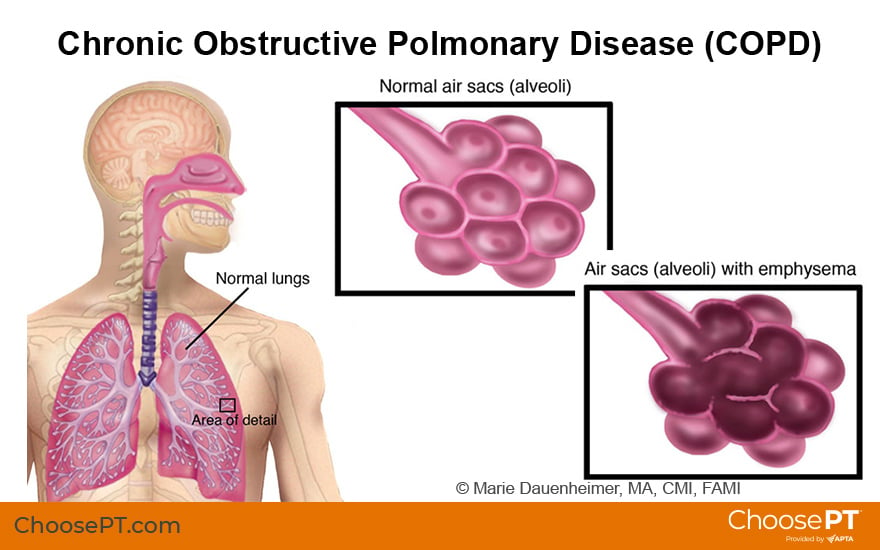
Emphysema. A condition in which small air sacs in the lungs called alveoli are damaged. The body has trouble getting all the oxygen it needs. This results in shortness of breath (dyspnea) and a chronic cough.
In addition to breathing problems, COPD can affect the whole body and lead to:
- Weakness.
- Balance problems.
- Increased risk of falls.
- Nutritional problems (weight loss or gain).
People with COPD are likely to have other health problems that can occur at the same time or be related to COPD. These problems can include:
- Reduced blood supply to the heart (ischemic heart disease).
- High blood pressure (hypertension).
- Depression.
- Lung cancer.
- Osteoporosis.
- Diabetes.
- Heart disease or heart failure.
- Atrial fibrillation.
- Asthma.
COPD leads to a decline in physical function due to increased shortness of breath and loss of muscle strength. There are four stages of COPD. They are determined by the amount or flow of air you can inhale and exhale. They are classified as:
- Mild.
- Moderate.
- Severe.
- Very severe.
People with COPD may need medications or supplemental oxygen.
How Is It Diagnosed?
Your health care provider can diagnose COPD through a variety of lung function tests. One important test is a spirometry test, which measures how much air you breathe out. Spirometry can detect COPD even before you notice symptoms of the disease.
How Can a Physical Therapist Help?
Your physical therapist will perform an evaluation that includes reviewing your health history. They may ask you questions such as:
- Do you smoke? If you quit smoking, how long did you smoke and how long has it been since you quit smoking?
- Have you had exposure to toxic chemicals or other pollution?
- Have you needed treatment in a hospital related to breathing problems?
- What medications are you taking?
- What makes your symptoms worse, and what relieves them?
Your physical therapist will review any lung function test results that may have been done by your doctor. They also will perform several tests to assess your condition. These may include:
- Muscle strength tests of your arms, legs, and core.
- Walking tests to measure your exercise capacity and activity tolerance.
- Tests of your balance and your risk of falling.
Research shows that pulmonary (lung) rehabilitation, including exercise training for at least four weeks, improves shortness of breath and quality of life. It also provides strategies for coping with COPD. Your physical therapist will serve as an important member of your health care team. They will work closely with you to design a program that considers your goals for treatment. Your physical therapist's goal is to help you continue your roles and activities at home, work, and in the community.
Your physical therapy treatment plan will include strategies to:
Improve your breathing. People with COPD often have shortness of breath and reduced strength in the muscles used to breath in air. Your physical therapist can help you train your breathing muscles to reduce shortness of breath and increase exercise capacity. They may teach you pursed lip and other special breathing techniques, which can help make each breath more efficient.
Improve your ability to be physically active. Your physical therapist will design an exercise program to train the muscles you use for movement. They also will help you strengthen your arm muscles to increase aerobic capacity and reduce shortness of breath. You may use equipment such as a recumbent bike, treadmill, or stepper to improve cardiovascular endurance.
Research shows that strength training in people with moderate to severe COPD increases muscle mass and overall strength. Your physical therapist will provide exercises to strengthen your arms and legs using resistance bands, weights, and weighted medicine balls.
Regular physical activity can benefit your physical, mental, and social health. It also can prevent or improve many chronic conditions, such as heart disease, diabetes, obesity, depression, and some cancers.
Improve your balance. The decrease in function and mobility that occurs in people with COPD can cause balance problems. It also can increase the risk of falls. People who need supplemental oxygen can be at a greater risk for falling. If balance testing shows that you are at risk for falling, your physical therapist can guide you through exercises to improve your balance and help you feel steadier on your feet.
Can This Injury or Condition Be Prevented?
One of the most important ways to prevent COPD is to stop smoking. Quitting smoking also can delay the onset of COPD or the worsening of breathing problems. If you smoke and have a cough or shortness of breath but tests don't yet show a decline in your lung function, you may be able to avoid a COPD diagnosis — if you stop smoking now! The American Lung Association offers an online Freedom From Smoking program for adult smokers. Your physical therapist can help you get in touch with local smoking cessation programs.
If you already have COPD, your physical therapist can guide you to help keep it from getting worse. They will show you how to continue an exercise program at home or at a gym after your physical therapy treatment. Continuing regular exercise after pulmonary rehabilitation for COPD helps slow the decline in quality of life and shortness of breath during everyday activities. Patients who continue exercising after completing a pulmonary rehabilitation program can maintain the gains they have made. However, research shows that people who stopped their exercise program had a major decline in their exercise endurance and physical function.
When a person has COPD and is overweight or obese, breathing can be even more difficult. Too much excess weight also can reduce your ability to exercise and decrease overall quality of life. Your physical therapist can help you manage your weight or prevent weight gain by designing an exercise program targeted to your current abilities. They also can refer you to a dietician for help with proper nutrition for a healthy lifestyle.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a variety of conditions and injuries. You may want to consider:
- A physical therapist who is experienced in treating people with pulmonary problems.
- A physical therapist who is a board-certified clinical specialist, or who completed a residency or fellowship in cardiovascular and pulmonary physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist:
- Get recommendations from family and friends or from other health care providers.
- Ask about the physical therapist's experience in helping people with COPD.
- Be prepared to describe your symptoms in as much detail as possible and say what makes your symptoms worse.
The American Physical Therapy Association believes that consumers should have access to information to:
- Inform their health care decisions.
- Prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for hypotonia. They report recent research and provide information on the standards of practice in the United States and worldwide. They link to a PubMed* abstract (which may offer free access to the full text) or to other helpful resources. You can read them to learn more or bring a copy to your health care provider.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy or diagnosis, management, and prevention of COPD. Updated 2023. Accessed April 2023. https://goldcopd.org/2023-gold-report-2/
Cheng SWM, McKeough ZJ, McNamara RJ, Alison JA. Pulmonary rehabilitation using minimal equipment for people with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Phys Ther. 2023;103(5):pzad013. Article Summary on PubMed.
Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269–1283. Article Summary on PubMed.
Li Y, Wu W, Wang X, Chen L. Effect of endurance training in COPD patients undergoing pulmonary rehabilitation: a meta-analysis. Comput Math Methods Med. 2022;2022:4671419. Article Summary on PubMed.
National Heart, Lung, and Blood Institute. What is COPD? Updated March 24, 2022. Accessed April 25, 2023. https://www.nhlbi.nih.gov/health/copd
Núñez-Cortés R, Padilla-Acevedo P, Vergara-Peña F, et al. Clinical assessment of balance and functional impairments in people with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis. ERJ Open Res. 2022;8(4):00164-2022. Article Summary on PubMed.
de Lima FF, Cavalheri V, Silva BSA, et al. Elastic resistance training produces benefits similar to conventional resistance training in people with chronic obstructive pulmonary disease: systematic review and meta-analysis. Phys Ther. 2020;100(11):1891–1905. Article Summary on PubMed.
Fiorentino G, Esquinas AM, Annunziata A. Exercise and chronic obstructive pulmonary disease (COPD). Adv Exp Med Biol. 2020;1228:355–368. Article Summary on PubMed.
Martí JD, McWilliams D, Gimeno-Santos E. Physical therapy and rehabilitation in chronic obstructive pulmonary disease patients admitted to the intensive care unit. Semin Respir Crit Care Med. 2020;41(6):886–898. Article Summary on PubMed.
Rutkowski S, Rutkowska A, Kiper P, et al. Virtual reality rehabilitation in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Int J Chron Obstruct Pulmon Dis. 2020;15:117–124. Article Summary on PubMed.
Adolfo JR, Dhein W, Sbruzzi G. Intensity of physical exercise and its effect on functional capacity in COPD: systematic review and meta-analysis. J Bras Pneumol. 2019;45(6):e20180011. Article Summary on PubMed.
Beaumont M, Forget P, Couturaud F, Reychler G. Effects of inspiratory muscle training in COPD patients: a systematic review and meta-analysis. Clin Respir J. 2018;12(7):2178–2188. Article Summary on PubMed.
Collinsworth AW, Brown RM, James CS, et al. The impact of patient education and shared decision making on hospital readmissions for COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1325–1332. Article Summary on PubMed.
Soriano JB, Polverino F, Cosio BG. What is early COPD and why is it important? Eur Respir J. 2018;52(6):1801448. Article Summary on PubMed.
Zeng Y, Jiang F, Chen Y, et al. Exercise assessments and trainings of pulmonary rehabilitation in COPD: a literature review. Int J Chron Obstruct Pulmon Dis. 2018;13:2013–2023. Article Summary on PubMed.
Expert Review:
Feb 25, 2023
Revised:
May 22, 2023
Content Type: Guide
Chronic Obstructive Pulmonary Disease (COPD)
PT, MS
Leonard D. Arguelles
PT, DPT, board-certified clinical specialist in cardiovascular and pulmonary physical therapy, on behalf of the APTA Academy of Cardiovascular and Pulmonary Physical Therapy
You Might Also Like...
Article
Cardiovascular and Pulmonary Physical TherapyJul 3, 2024
Learn about the knowledge, experience, and expertise of physical therapists who focus on or specialize in cardiovascular and pulmonary physical
Podcast
Pulmonary Conditions and the Role of Physical TherapyJul 11, 2013
July 11, 2013: A physical therapist discusses the role of physical therapy in treating conditions such as asthma, cystic fibrosis, COPD, and more.
