Physical Therapy Guide to Temporomandibular Disorder
Temporomandibular disorder, or TMD, is a common condition that affects people of all ages and genders. Women of childbearing age are affected three times more than men. TMD can involve problems with the joints of the jaw (temporomandibular joint, or TMJ) or the muscles that move the jaw. For those with persistent TMD, it is common to have both muscle and joint problems. Symptoms of TMD can include jaw pain, difficulty fully opening the mouth, locking of the jaw, and painful "crackling" or "popping" noises with jaw movement. TMD is often linked with neck pain. Other symptoms beyond the face may include earache, ear ringing, headache, dizziness, and problems with swallowing. A range of problems can cause TMD, such as trauma from dental work, a car accident, or a blow to the face. However, TMD also can result from chronic teeth clenching and grinding, neck and face tension from stress and poor posture, or faulty movement patterns.
Conservative management, including physical therapy, is the recommended first-line approach for TMD. A team approach to treating TMD, which may involve other health issues, is important for successful management. This is especially true when problems are persistent. Physical therapists use an evidence-based approach to evaluate and treat TMD, aimed at providing people with the tools to manage symptoms and improve function.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is Temporomandibular Disorder?
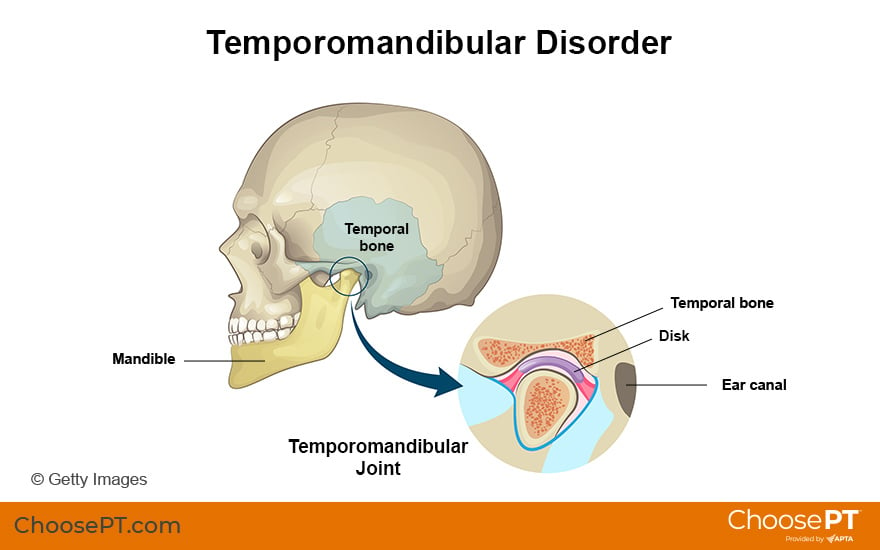
The temporomandibular joint, or TMJ, is a hinge joint. It is located in front of your ear and connects your jaw to your skull. The TMJ functions to open and close the mouth and move the jaw from side to side and front to back. It allows you to chew, swallow, and talk. TMD occurs when the natural function of the TMJ is altered or limited due to disturbance of the joint itself or the ligaments or muscles in the head, neck, and face area.
Causes of TMD include:
- Trauma. Examples of trauma include:
- A lengthy dental procedure.
- Motor vehicle accident.
- Blow to the face and jaw.
- Poor head and neck posture.
- Clenching and grinding the teeth at night.
- Muscle tightness due to stress.
- Chronic jaw clenching or grinding (bruxism). Many people clench their jaws or grind their teeth during sleep. This is an involuntary behavior (done without thinking). Some people also clench their teeth during the day, especially when under stress. Wearing a night splint may help decrease the degree of clenching and prevent the wear and tear of your teeth. Stress management has been proven effective in controlling this behavior.
- Poor posture habits. A forward-head posture during activities, such as sitting, standing, cooking, and computer or cell phone use, may lead to tightness in the jaw and neck muscles. This can result in TMD.
- Abnormal teeth alignment (malocclusion). This may affect the normal function of the TMJ due to an inadequate chewing pattern.
- Jaw fracture. A broken jaw due to an accident or surgery will affect the function of TMJ.
- Surgery. Pain, stiffness, and limited mouth opening after jaw or facial surgery may lead to TMD. A physical therapist skilled in treating people with TMD can help you restore proper jaw movement after surgery to the face, mouth, or jaw.
- Trismus (lockjaw). A muscle spasm of the jaw after a lengthy dental procedure will limit your ability to open your mouth.
- Displacement of the disc or soft-tissue cushion located between the ball and socket of the TMJ. This condition causes popping or clicking of the jaw and often leads to pain, and limits your ability to open your mouth.
- Arthritis. Osteoarthritis, linked to joint overuse, can destroy the soft-tissues and change the shape and function of the jaw. Inflammation from rheumatoid arthritis, which causes the immune system to attack healthy tissue, and psoriatic arthritis, can damage the jaw.
How Does It Feel?
TMD can be temporary or last for years. People with TMD may experience:
- Jaw pain (the most common symptom).
- Difficulty opening the mouth fully.
- Shifting of the lower jaw to one side at the end of mouth opening. The jaw also may move from side to side during opening.
- Pain with chewing certain foods.
- Noises in the jaw (crackling or popping) with chewing or talking.
- Headaches.
- Neck or facial pain.
- Dizziness.
- Earache, stuffy ear, or ringing in the ear.
- Jaw fatigue.
- Lockjaw. The jaw gets stuck in a partly open position.
- Difficulty swallowing.
- Problems with speaking.
- Anxiety or a sense of helplessness.
Caution: Jaw pain also can be a symptom of a heart attack. Seek medical care immediately if you have jaw pain, along with any of the following symptoms:
- Chest pain.
- Shortness of breath.
- Dizziness.
- Pain in the left arm.
- Numbness in the left arm.
- Nausea.
How Is It Diagnosed?
After taking a detailed history of your condition, your physical therapist will evaluate your head, neck, and TMJ. They also will assess:
- Your posture.
- Breathing pattern.
- Stress level.
- Other factors that may contribute to your condition.
Your physical therapist will determine whether the cause of your specific condition is joint- or soft-tissue-related, or a combination.
If your physical therapist suspects your teeth alignment may be causing your TMD, they will refer you to a dentist or orthodontist for further evaluation. You may benefit from a night splint.
How Can a Physical Therapist Help?

Your physical therapist can help you decrease your pain and restore jaw function. They will design a treatment program for your specific condition. Your physical therapy program may include:
- Education. Your physical therapist will discuss the cause of your TMD and educate you about:
- Proper posture and body mechanics.
- Tongue resting position.
- Eating a soft diet when appropriate.
- Exercise.
- A self-management routine.
Patient education aims to reduce your discomfort and prevent future aggravation and symptoms.
- Modalities. Your physical therapist will determine which treatments are best for you. These may include using treatments such as heat or ice, ultrasound, electrical stimulation, light therapy, or other tools to prepare your soft-tissue for manual (hands-on) therapy.
- Soft-tissue release. Your physical therapist may use hands-on treatments to mobilize your soft-tissue. This can address muscle spasms and tightness. They may work on your face and jaw and inside your mouth.
- Joint mobilization. Your physical therapist will address any stiffness in your neck and jaw to help restore movement of your TMJ.
- Therapeutic exercises. Your physical therapist will teach you specific exercises to repeat several times throughout the day. Doing them can help you break the cycle of pain and spasm. These exercises will help address imbalances in the involved muscles and improve joint mobility to support and keep proper alignment of your head, neck, and jaw.
- Stress management. Your physical therapist can teach you ways to help you manage stress and offer psychological support and positive encouragement. If needed, they will refer you to a psychologist or other appropriate health care provider.
If Surgery Is Needed
If you need surgery, a physical therapist can provide a pre-surgery program. Before surgery, your physical therapist will educate you about the procedure and what to expect afterward. They will record a baseline measurement of your joint mobility and provide you with a proper exercise program and positive support.
After surgery, your physical therapist will provide treatment for pain relief, soft-tissue release, and joint mobilization. They will design a graded exercise program and functional training to help you recover and restore your jaw to full function.
Can This Injury or Condition Be Prevented?
You can prevent TMD by maintaining proper head and neck posture, learning how to manage stress, and addressing muscle tightness when it occurs.
A physical therapist can help you avoid a recurrence or worsening of TMD symptoms by educating you on:
- How to sit, stand, and work with a proper posture.
- Avoiding clenching the jaw during the day.
- Ways to release muscle tightness through heat, massage, and stretching.
- Specific daily exercises to support your head, neck, and TMJ.
- Stress management techniques.
- How to maintain a healthy aerobic exercise program.
General tips for people with TMD include:
- Maintain a good posture at all times. Avoid slouching in front of the computer or when checking phone messages.
- Keep your tongue on your palate (roof of the mouth), with your lips closed and your teeth apart while breathing naturally.
- Chew only soft foods when pain is severe.
- Avoid eating foods that are hard (such as tough meat, bagels), chewy (such as gum, candies), or crunchy (such as salad or chips).
- Avoid opening the jaw too wide during activities like yawning, laughing, or singing.
- Avoid smoking.
- Maintain good oral hygiene and tooth health.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to identify TMD and provide appropriate treatment. However, you may want to consider:
- A physical therapist who has training in managing TMD. You may want to see a physical therapist with clinical expertise in the head/neck/TMJ area.
- A physical therapist who is a board-certified clinical specialist or who has completed a residency or fellowship in orthopedic physical therapy. This physical therapist has more advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists in your area who have these and other credentials by using Find a PT, a tool built by the American Physical Therapy Association.
General tips when you are looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- Ask about the physical therapist’s experience in helping people with TMD before making an appointment.
- Be prepared to describe your symptoms in as much detail as possible.
The following articles provide the best scientific evidence for how to treat TMD. The articles report recent research and give an overview of the standards of practice for TMD treatment in the United States and internationally. The article titles are linked either to a PubMed abstract of the article or free full text so that you can read it or print out a copy to bring with you to your health care provider.
Garrigos-Pedron M, Elizagaray-Garcia I, Dominguez-Gordillo AA, et al. Temporomandibular disorders: improving outcomes using a multidisciplinary approach. J Multidiscip Healthc. 2019;12:733–747. Article Summary on PubMed.
Hong SW, Lee JK, Kang JH. Relationship among cervical spine degeneration, head and neck postures, and myofascial pain in masticatory and cervical muscles in elderly with temporomandibular disorder. Arch Gerontol Geriatr. 2019;81:119–128. Article Summary on PubMed.
Huttunen J, Qvintus V, Suominen AL, Sipila K. Role of psychosocial factors on treatment outcome of temporomandibular disorders. Acta Odontol Scand. 2019;77(2):119–125. Article Summary on PubMed.
Lindfors E, Arima T, Baad-Hansen L, et al. Jaw exercises in the treatment of temporomandibular disorders-an international modified Delphi study. J Oral Facial Pain Headache. 2019;33(4):389–398. Article Summary on PubMed.
Dickerson SM, Weaver JM, Boyson AN, et al. The effectiveness of exercise therapy for temporomandibular dysfunction: a systematic review and meta-analysis. Clin Rehabil. 2017;31(8):1039–1048. Article Summary on PubMed.
List T, Jensen RH. Temporomandibular disorders: old ideas and new concepts. Cephalalgia. 2017;37(7):692–704. Article Summary on PubMed.
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Expert Review:
May 14, 2022
Revised:
Mar 4, 2025
Content Type: Guide
Temporomandibular Disorder
PT, DPT, board-certified clinical specialist in orthopaedic physical therapy
Stephen F. Reischl
PT, DPT, board-certified clinical specialist in orthopaedic physical therapy, on behalf of the Academy of Orthopaedic Physical Therapy.