Physical Therapy Guide to Total Hip Replacement (Arthroplasty)
Total hip replacement (arthroplasty) is a common surgical intervention that is performed for severe arthritis or hip fracture when conservative treatments are ineffective. The goal of total hip replacement surgery is to relieve pain, improve joint mobility, and restore or improve a person’s ability to safely perform functional activities like walking, standing, stair climbing, or running. Physical therapists work with people who have had a total hip replacement to strengthen their muscles and restore movement to their highest potential.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is Total Hip Replacement (Arthroplasty)?
Total hip replacement surgery removes damaged bone and cartilage that may be contributing to a painful, dysfunctional hip, and replaces the damaged hip with a prosthetic (artificial) hip.
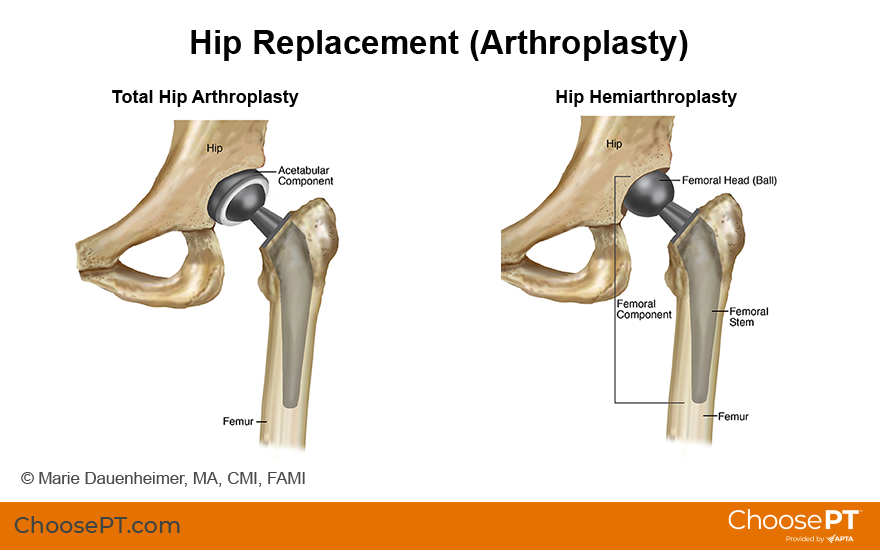
The hip joint is a ball-and-socket joint. The ball is part of the femur (thigh bone) and the socket is part of the hip bone/pelvic bone. The type of hip replacement surgery performed varies with each individual's physical condition.
The 2 types of hip replacement surgeries are:
Total Hip Replacement (Arthroplasty)
With total hip replacement (arthroplasty), the ball and the socket are both replaced with artificial parts. Total hip replacement is performed to treat conditions including:
- Osteoarthritis of the hip
- Rheumatoid arthritis
- Traumatic arthritis
- Ankylosing spondylitis
- Avascular necrosis (loss of bone tissue)
- Certain hip fractures
- Benign and malignant tumors
Partial Hip Replacement (Hemiarthroplasty)
A partial hip replacement (hemiarthroplasty) only replaces the ball of the hip joint; the hip socket remains strong and doesn’t need to be replaced. Hemiarthroplasty is performed when there is damage only to the “femoral” or thigh portion of the hip joint. This is mostly performed in patients who are elderly and frail, and for fractures involving the ball or the neck of the femur (thigh bone).
How Does It Feel?
Before surgery, people who have elected to undergo total hip replacement may describe severe pain in the hip and groin that can extend down the thigh. The pain may significantly affect a person’s ability to walk, climb stairs, sit down or stand up, perform daily activities, and sleep on the affected side.
Immediately after total hip replacement surgery, you will experience stiffness in the hip and leg, and muscle weakness. Initially, pain is managed primarily with medication. Your physical therapist also may recommend ice packs to help reduce discomfort and swelling, and teach you gentle exercises and movements to begin to improve your motion and strength.
How Is It Diagnosed?
To be considered for a total hip replacement, most individuals will have already been seen by a medical professional. Your physician will order x-rays to assess whether there are changes to the bones and cartilage of your hip. If you have had a fall, x-rays will also guide the attending health care professionals in determining if there is a fracture and if it requires surgery in order for you to regain your function. A physical therapist will evaluate your range of motion, strength, and how much your hip pain impacts your functional mobility. Factors can include how you get in and out of bed, sit down and stand up, squat down, walk, and navigate stairs and curbs. The results of these evaluations will help determine whether you might benefit from total hip replacement surgery.
Hip replacements are most often performed in adults aged 60 to 80 years. Your medical team will help you determine if you are a good candidate for surgery based on your x-rays and your physical assessment. Risk factors that may interfere with your recovery, such as advanced age, obesity, or a history of smoking or excessive alcohol use will be taken into account.
How Can a Physical Therapist Help?
Before Surgery
Your physical therapist can help educate you about what to expect from your surgery, and give you exercises to condition your body before surgery.
In preparation for surgery, your physical therapist may teach you:
- Flexibility and strengthening exercises for the lower extremities
- How to use a walker or crutches for walking and for navigating steps
- Any precautions to take after surgery
Your physical therapist also may recommend that you make changes in your home to improve safety and help your recovery, including the use of a raised toilet seat, handrails on stairs, a bed rail, and a tub seat or grab bars in the shower. These changes ideally should be made before you have surgery, so your home is prepared for your return.
After Surgery
On the first or second day after your surgery, a physical therapist will come to your bedside to begin your postoperative treatment. Your physical therapist will review any postsurgical precautions to take to prevent reinjury and to help restore your full function.
Depending on your particular case/surgical procedure, you may be asked to limit the amount of weight you put on the surgical leg. It may be as little as a toe touch, or as much weight bearing as you can tolerate. Your physical therapist will teach you how to correctly put weight on the affected leg, and will recommend an assistive device, such as a walker or crutches, to minimize discomfort as you work to restore your physical function.
During your acute-care recovery (the first 3 to 5 days after surgery), your physical therapist will work with you to help you safely:
- Turn in bed and get up to a sitting position.
- Get out of bed to stand and move to a chair.
- Walk with the assistive device (walker or crutches) for short distances.
- Perform gentle range-of-motion and strengthening exercises in bed.
After surgery, your physical therapist may advise you not to:
- Bend your new hip more than 90°.
- Bend forward more than 90° (eg, you will not be able to bend over to put on your socks and shoes for a while).
- Cross your leg with your new hip over the other leg.
- Turn the leg with the new hip inward.
Physical therapy will continue for a number of weeks after your surgery. Depending on your overall situation, you may need to recover in a short-term rehabilitation facility. Some patients are discharged to their home without nursing home care, depending on the help available at home and their ability to stay safe. Your physical therapist will help make this determination for you.
As you progress in your recovery, you will continue to work on:
- Walking and stair climbing
- Balance – after surgery your balance may be impaired, which could put you at risk for falls
- Transferring to the bed, a chair, and a car
- Full movement of your leg and new hip (such as putting on socks and shoes)
- Specific muscle strengthening exercises to improve your ability to stand and walk safely and independently
When you can perform these activities without help or guidance, you will be ready to fully function at home. However, you may still need to continue physical therapy in an outpatient clinic.
Outpatient physical therapy sessions will continue your work on range-of-motion (movement) and stretching exercises, and weight-bearing activities to restore your function to its highest possible level. At this point, your physical therapy will focus on activity-specific rehabilitation for your specific goals, such as a return to work or sport. Your physical therapist will incorporate exercises that simulate those activities. Your exercise regimen may include lifting techniques, pushing, pulling carts, climbing ladders, agility exercises, or light jogging, depending on your specific goals, your recovery progress, and your activity level.
Can This Injury or Condition Be Prevented?
It may be possible to prevent or slow the onset of osteoarthritis, a condition that can require total hip replacement surgery, by choosing a healthy lifestyle, such as participating in regular exercise and eating a healthy diet. Your physical therapist can teach you conditioning, strengthening, and flexibility exercises to help you maintain peak fitness throughout your life span.
More than 95% of hip fractures are caused by falls. The best way to prevent the need for unplanned total hip replacement surgery is to prevent a fall. Your physical therapist can help you reduce your chances of falling by evaluating your fall risk and prescribing balance activities and regular weight-bearing exercises. Your physical therapist also can recommend changes in your home environment to improve your safety, such as removing trip hazards like unstable rugs, or adding grab bars in the bathroom.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a variety of conditions or injuries. You may consider the following when you are looking for a physical therapist:
- A physical therapist who is experienced in treating patients with orthopedic or musculoskeletal conditions.
- A physical therapist who has experience in treating patients after a total joint replacement.
- A physical therapist who is a board-certified specialist in orthopedics.
You may use the online search tool Find a PT located on the American Physical Therapy Association's website to locate a physical therapist in your area.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, from other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience with total hip replacement surgery.
- During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible.
- You may also ask friends or family for advice if they have attended physical therapy in the past.
The American Physical Therapy Association believes that consumers should have access to information that could help them make health care decisions and also prepare them for a visit with their health care provider.
APTA has determined that the following articles provide some of the best scientific evidence on total hip arthroplasty. The articles report recent research and give an overview of the standards of practice for treatment both in the United States and internationally. The article titles are linked either to a PubMed* abstract of the article or to free access of the full article, so that you can read it or print out a copy to bring with you to your health care provider.
Cibulka MT, Bloom NJ, Enseki K, et al. Hip pain and mobility deficits–hip osteoarthritis: revision 2017. J Orthop Sports Phys Ther. 2017;47(6):A1-A37. Free Article.
Nanaku M, Tsuboyama T, Akiyama H, et al. Preoperative prediction of ambulatory status at 6 months after total hip arthroplasty. Phys Ther. 2013;93:88–93. Article summary in PubMed.
Slaven EJ. Prediction of functional outcome at six months following total hip arthroplasty. Phys Ther. 2012;92:1386-1394. Article summary in PubMed.
Vissers MM, Bussmann JB, Verhaar JA. Recovery of physical functioning after total hip arthroplasty: systematic review and meta-analysis of the literature. Phys Ther. 2011;91:615-629. Article summary in PubMed.
*PubMed is a free online resource developed by the National Center for Biotechnology Information (NCBI). PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine's MEDLINE database.
Expert Review:
Sep 25, 2018
Revised:
Sep 25, 2018
Content Type: Guide
Hip Replacement
PT, DPT, a board-certified clinical specialist in orthopaedic physical therapy
Pranjali Sathe
PT, DPT, board-certified clinical specialist in orthopaedic physical therapy
Jennifer Halvaksz
PT, DPT, a board-certified clinical specialist in orthopaedic physical therapy
You Might Also Like...
Did You Know?
Prescribed Opioids Resulted in 3.3 Billion Unused PillsNov 1, 2017
Despite increased efforts and awareness to reduce opioid use after surgery, nine out of 10 patients were prescribed an average of 85 pills after surgery
Podcast
Success Story: An Art Teacher's Journey to a Pain Free LifeSep 1, 2016
Joanne was enjoying life as an art teacher when she started having hip pain that intensified, making it hard to stand or walk.
Podcast
Total Hip ReplacementJun 5, 2014
The Centers for Disease Control and Prevention estimates that 25% of people may develop hip osteoarthritis by age 85.

