Physical Therapy Guide to Stroke
Stroke occurs when a blood vessel in the brain is blocked or ruptures and the blood flow in the brain stops. Stroke is the third leading cause of death in the United States. It also is a leading cause of serious and long-term disability. A stroke can happen at any time to people of any race, gender, or even age. More women than men have a stroke each year. African Americans have almost twice the risk of a first-time stroke as Caucasians. About two-thirds of those who experience a stroke are over age 65. Nearly 800,000 people in the U.S. have a stroke each year.
Physical therapists provide treatments for people who have had a stroke to restore movement and walking ability, decrease disability, and improve function.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is Stroke?
Stroke is also called a cerebral vascular accident. Stroke occurs when a blood vessel in the brain is blocked (blood flow in the brain stops) or ruptures. It is an emergency. Blood carries a constant supply of oxygen and nutrition that the brain requires. When the blood flow in the brain is interrupted, a part of the brain does not receive enough oxygen and nutrition. This causes damage as the brain cells begin to die within a few minutes. The amount of brain cell death depends on the severity and duration of the blockage or rupture. The functions controlled by the areas with dead or damaged brain cells may be lost or limited. This may include losing the ability to:
- Move, walk, or use the hands.
- Speak or think.
- Control the bowel, bladder, and other body functions.
Delaying treatment increases the risk of permanent brain damage, disability, or death.
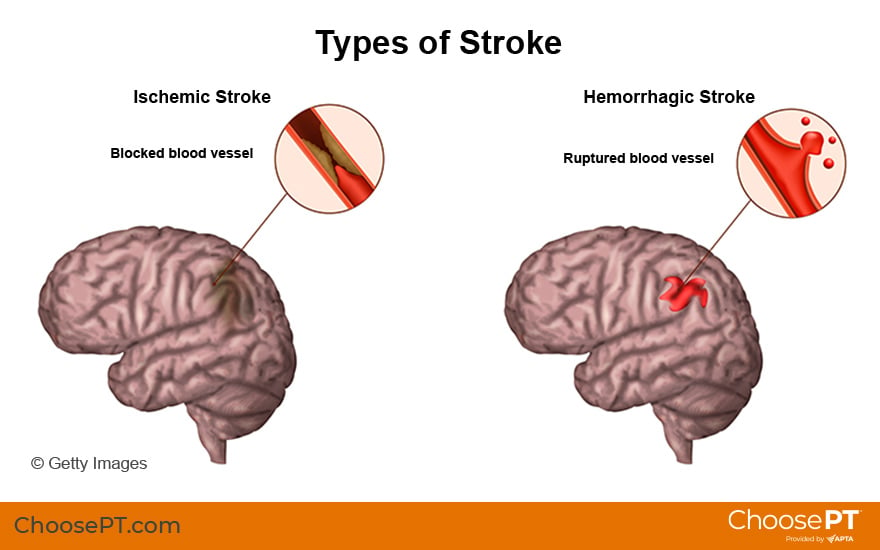
There are two types of stroke:
An ischemic stroke is the most common type. It occurs when a blood vessel is blocked. A blood clot or a buildup of fatty deposits (arteriosclerosis) in the blood vessels that supply the brain can lead to blocked blood vessels. Ischemic stroke accounts for 87% of all strokes. The most common cause of ischemic stroke is fatty deposits lining the blood vessel walls.
A hemorrhagic stroke occurs when a weakened blood vessel leaks or ruptures. When a blood vessel bursts in the brain, blood builds up and damages surrounding brain tissue. The most common cause of hemorrhagic stroke is high blood pressure. Hemorrhagic stroke also can occur in people with a tangle of abnormal vessels connecting arteries and veins in the brain. This tangle is called brain arteriovenous malformation. AVM may disrupt blood flow and result in bleeding in the brain.
Both types of stroke damage brain cells. The damage causes symptoms that start to show in the parts of the body and functions controlled by those brain cells.
How Does It Feel?
A stroke is a serious medical condition that requires emergency care. It is important to know the signs of a stroke and get help quickly if you or someone you are with shows any signs of stroke. Medical treatment is most effective when started immediately.
If you have one or more of the following symptoms, call 911 right away for an ambulance:
- Sudden numbness or weakness of the face, arm, or leg, especially on one side of the body.
- Sudden confusion or trouble speaking or understanding.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble moving or walking.
- Sudden dizziness or loss of balance or coordination.
- Sudden, severe headache with no known cause.
- Sudden nausea or vomiting not caused by infection or viral illness.
- Loss or change of consciousness, confusion, or seizures with no known cause.
Emergency treatment with a clot-buster drug called t-PA can help reduce or even eliminate problems from stroke. The drug must be given within three hours of when symptoms start.
Act FAST
The acronym FAST is an easy way to remember the signs of a stroke. If you think someone might be having a stroke, act FAST and call 911.
FAST stands for:
F=Face. Ask the person to smile. Does one side of the face droop?
A=Arms. Ask the person to raise both arms. Does one arm drift downward?
S=Speech. Ask the person to repeat a simple phrase. Does the speech sound slurred or strange?
T=Time. If you observe any of these signs, call 911 at once and note the time that you think the stroke began.
Research shows that people with stroke who arrive at the hospital by ambulance receive quicker treatment than those who arrive by their own means.
Awareness of stroke symptoms and calling 911 are vital to enable emergency medical personnel to quickly begin stroke care and deliver advanced treatment as soon as possible.
Signs and Symptoms
Stroke symptoms may happen suddenly. The symptoms may vary from one person to another. Symptoms may include:
- Sudden numbness or weakness of the face, arm, or leg, especially on one side of the body.
- Confusion about where you are or what you're doing.
- Trouble speaking or understanding what others are saying.
- Trouble seeing in one or both of your eyes.
- Trouble walking, dizziness, or loss of balance.
- A sudden, severe headache that seems to come out of nowhere.
- Sudden nausea or vomiting not caused by infection or viral illness.
- A sudden loss or change of consciousness, confusion, or seizures with no known cause.
Some people experience a transient ischemic attack, called a ministroke, that produces stroke-like symptoms. TIAs do not cause permanent damage because blood flow is altered for only a short time (from a few minutes to up to 24 hours). Recognizing symptoms and seeking treatment for TIAs can reduce your risk of a major stroke.
Stroke can cause a range of long-term problems, such as:
- Trouble moving or not being able to move one side of the body.
- Severely limited movement or stiffness in the arms and legs.
- Balance problems.
- Weakness on one side of the body.
- Off-and-on numbness.
- Loss or lack of sensation (feeling).
- Sensitivity to cold.
- Memory loss.
- Slowed or slurred speech.
- Problems remembering words.
How Is It Diagnosed?
Getting diagnosed early is linked to better outcomes for people who experience a stroke. Physicians or emergency medical personnel will assess a stroke based on the signs and symptoms. They typically consider the FAST signs for stroke. Doctors often confirm a stroke diagnosis by examining the patient, using specific tests, and taking images of the brain (usually a CT scan or MRI). The diagnosis of stroke is most difficult in the initial hours, particularly when:
- The onset is uncertain.
- Symptoms are changing or atypical.
- The patient is agitated.
- There is a delay in access to imaging.
- Brain imaging is normal or doesn’t appear to show any brain lesion.
Research has proven that early treatment can reduce the effects of stroke and save lives. Efforts are being made to get people suspected of having a stroke directly to a hospital stroke unit rather than the emergency department.
How Can a Physical Therapist Help?
Physical therapists are part of the stroke recovery team. Physical therapy begins very soon after a stroke, most often while you are still in the hospital. Your physical therapist’s main goal is to help you return to your activities at home, at work, and in your community.
Evaluation is very important for guiding the treatment of stroke. Your physical therapist will conduct a thorough assessment that includes:
- Taking a health history.
- Discussing your symptoms in detail.
- Detecting risk factors associated with the condition.
- Reviewing lab tests and X-rays or other images.
- Observing your ability to move, stand, walk and do other movements.
- Conducting a hands-on physical assessment.
After conducting an exam and evaluating your condition, your physical therapist will develop a treatment plan specific to your needs, challenges, and goals. They will work with you to help you achieve the best possible quality of life. Your treatment plan will focus on:
- Improving your ability to move.
- Addressing any pain you might have.
- Offering guidance on ways to prevent problems that may occur after a stroke.
One of the first things your physical therapist will teach you is how to move safely from your bed to a chair and do exercises while in bed. As you become more mobile, your physical therapist will teach you strengthening exercises and functional activities.
Later, your physical therapist will:
- Help you improve your balance and walking ability.
- Fit you with a brace or a wheelchair, if needed.
- Provide training to your family and caregivers.
- Teach you how to use devices that can help you stay mobile when a stroke has affected your ability to move, walk, or keep your balance. These can include orthoses, prostheses, canes, walkers, wheelchairs, and perhaps even robotics.
Treatment for people with stroke varies. Your specific treatment will depend on the results of your physical therapist's evaluation and on how long it's been since your stroke. Recovery from a stroke depends on:
- The size and location of your stroke.
- How quickly you received care.
- The severity of the brain damage at the time of your stroke.
- Your other health conditions.
Your physical therapist will help you regain functional skills to allow you to take part in your specific life activities.
Relearning How To Use Your Upper Body, Walk, and Perform Daily Activities
Your physical therapist will design an exercise and strengthening program based on tasks you need to do every day. Physical therapist researchers are at the forefront of innovating many techniques for stroke recovery. Your physical therapist will select the best treatment for your specific needs from a variety of available options, such as:
- Task-oriented and functional training. This type of training allows a person to practice tasks and functional activities they do in real-life situations. This can include activities such as getting up from a chair, walking, and climbing stairs.
- Strength training. Strength training can include traditional strength training that uses weights or a functional strength-training approach. Functional strength training involves practicing real-time tasks. For example, rising from a chair several times can be used to strengthen leg muscles. Reaching toward objects several times can be used to strengthen the arm muscles.
- Walking and balance training. Physical therapists use different training methods to help improve balance and walking. Balance training involves practicing activities that challenge balance. Gait training involves activities that help a person relearn how to walk and improve walking patterns. These may include bearing weight on the affected leg, walking on a treadmill, stepping onto a stair, and walking over different surfaces.
- Constraint-induced movement therapy. Physical therapists use CIMT to strengthen a person’s arm that is affected by stroke. They will apply a mitten or a sling on your strong arm to keep you from fully using it. This constraint requires you to use the arm or hand affected by the stroke to perform daily tasks to help build back strength and control.
- Functional electrical stimulation. This treatment uses small electrical pulses to activate nerves and make weakened muscles move. It can help improve movement and enhance control in limbs affected by stroke.
- Motor imagery and mental practice. This technique uses tools to help strengthen the arms, hands, feet, and legs. Working with your physical therapist, you will "rehearse" a movement without actually performing it. This practice stimulates the part of your brain that controls the desired movement.
- Positioning. Proper positioning helps reduce any muscle pain, spasms, slowness, or stiffness resulting from stroke. Your physical therapist will teach you how to safely move (transfer) from a sitting to a standing position. They also will show you how to properly support yourself when sitting or lying down, using foam wedges, slings, and other aids.
- Robotic, virtual reality, and interactive video games. These tools provide experiences that mimic real-life activities and situations. Your physical therapist will help you use a smart device or a robotic device to practice daily tasks. These exercises help to "rewire" your brain and nerve connections. Your physical therapist may teach you how to continue these activities at home.
- Body weight support. BWS is used to carry some of your weight and help support you as you walk, usually on a treadmill. Your physical therapist will gradually decrease the amount of support as your posture, strength, balance, and coordination improve.
- Biofeedback. This treatment helps make you aware of how your muscles work and how you might gain better control over them. Your physical therapist will attach electrodes to your skin to display measurements of your muscle activity on a monitor. They will work with you to help you understand and change those readings.
Your needs will change over time, and your physical therapist may consider using other treatments and tools to assist you in your recovery, such as:
- Aquatic therapy.
- Robotics.
- Braces.
- Support devices such as different types of walkers and canes.
Even after the initial recovery phase in a rehabilitation facility, your physical therapist will continue to see you as needed to:
- Assess your progress.
- Update your exercise program.
- Help you prevent further problems.
- Promote the healthiest possible lifestyle.
Can This Injury or Condition Be Prevented?
The American Stroke Association estimates that 80% of strokes can be prevented. Some risk factors for stroke can't be changed. These include:
- Family history.
- Age.
- Gender.
- Race (stroke death rates are higher for African Americans, even at younger ages).
- Previous heart attack or stroke.
However, you can reduce many causes of stroke by making lifestyle changes. To reduce your risk for stroke:
- See a doctor for a checkup and measure your blood pressure regularly to check for high blood pressure. Take your medication as prescribed. High blood pressure causes about one-half of all strokes.
- Quit smoking. If you are a smoker, join a program to help you quit. The Centers for Disease Control and Prevention offers resources for quitting.
- Reduce high cholesterol by following your doctor’s recommendations.
- Manage diabetes by following your doctor’s recommendations. Eat a healthy diet, get the recommended amount of daily physical activity, and take prescribed medication.
- Get treatment if you have been diagnosed with carotid artery disease.
- Engage in daily physical activity for general health and to reduce obesity. Your physical therapist is an expert at designing a health and wellness activity plan specific to you.
- Reduce your alcohol intake.
Promoting heart health and managing stroke risk factors are central to preventing and managing stroke.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a variety of conditions or injuries. You may want to consider:
- A physical therapist who is a board-certified clinical specialist in neurology (called NCS) or who completed a residency or fellowship in neurologic physical therapy. This therapist has advanced knowledge, experience, and skills that may apply to your condition.
- A physical therapist who is experienced in treating people with problems related to stroke. Some physical therapists have a practice with a neurologic focus.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people with stroke.
- During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and say what makes your symptoms worse.
The American Physical Therapy Association believes that consumers should have access to information to help them make informed health care decisions and prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for survivors of stroke. They report recent research and give an overview of the standards of practice both in the United States and internationally. They link to a PubMed* abstract that also may offer free access to the full text, or to other resources. You can read them or print out a copy to bring with you to your health care provider.
Centers for Disease Control and Prevention. Stroke facts. Accessed April 12, 2021.
Stroke Association; American Heart Association. Heart disease and stroke statistics (2022 update). Accessed April 5, 2022.
American Stroke Association; American Heart Association. Post-stroke care. Accessed April 5, 2022.
Centers for Disease Control and Prevention. I'm ready to quit! Smoking cessation programs. Accessed April 12, 2021.
Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;3;141(9):e139–e596. Article Summary on PubMed .
Adeoye O, Nyström KV, Yavagal DR, et al. Recommendations for the establishment of stroke systems of care: a 2019 update. Stroke. 2019;50:e187–e210. Article Summary on PubMed.
Churilov I, Churilov L, MacIsaac RJ, Ekinci EI. Systematic review and meta-analysis of prevalence of sarcopenia in post acute inpatient rehabilitation. Osteoporos Int. 2018;29(4):805–812. Article Summary on PubMed .
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–e110. Article Summary on PubMed.
Hankey GJ. Stroke. Lancet. 2017;389(10069):641–654. Article Summary on PubMed.
Higashida R, Alberts MJ, Alexander DN, et al. Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke. 2013;44:2961–2984. Article Summary on PubMed.
PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Expert Review:
Apr 23, 2021
Revised:
Apr 23, 2021
Content Type: Guide
Stroke
PT, PhD, FAPTA
an academy of the American Physical Therapy Association
Yasser Salem
PT, MS, PhD, board-certified clinical specialist in neurologic and pediatric physical therapy, on behalf of APTA Neurology, an academy of the American Physical Therapy Association
You Might Also Like...
Article
Neurologic Physical TherapyJul 9, 2024
Neurologic physical therapists evaluate and treat conditions caused by nervous system diseases or injuries. They care for people of all ages and work with
Patient Stories
Physical Therapy Helps Young Man Chase His Dreams After Traumatic Brain InjuryJul 29, 2021
"I would not be where I am today if it were not for my physical therapists."
Podcast
Early Physical Therapy A Life Changer For Toddler After a Perinatal StrokeMay 6, 2021
A mother driven to help her infant son discovers the Early Intervention Program and fought to get him access to therapies that helped him thrive and keep


