Physical Therapy Guide to Below-Knee Amputation (Transtibial Amputation)
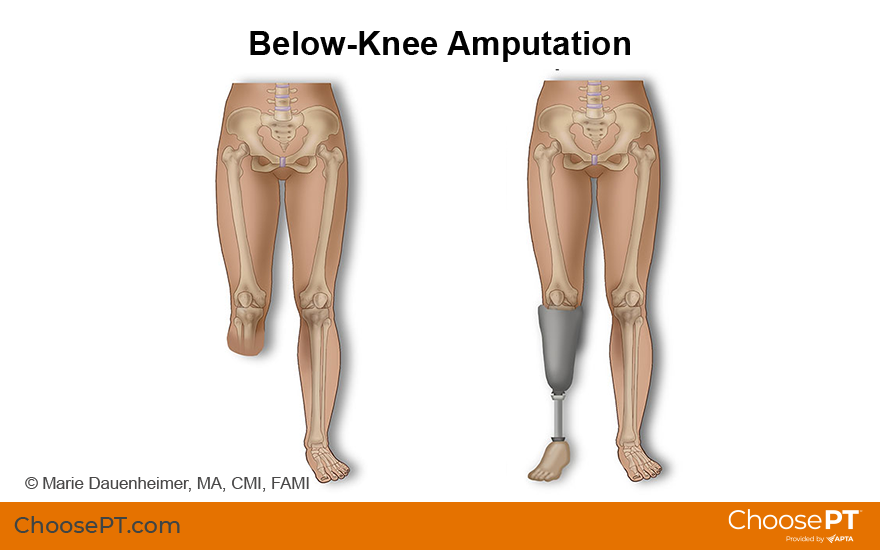
Transtibial amputation, or below-knee amputation, is a surgical procedure to fully remove a lower limb (leg). It is done when the leg has been damaged due to trauma, congenital defect, or disease. Below-knee amputation makes up 28% of all leg amputations. Amputation is possible at any age but is most common among people 65 years and older.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Causes Below-Knee Amputation?
Transtibial amputation is a surgical procedure to remove the leg below the knee. This surgery is done when the leg is severely damaged or diseased. Most below-knee amputations (70%-95%) are due to poor blood circulation, known as peripheral vascular disease. PVD limits healing and the body's immune response to injury and may lead to foot or leg ulcers. These ulcers may not heal and may develop an infection that can spread to the bone and become life-threatening. Amputation is performed to remove the diseased tissue and prevent the further spread of infection.
Amputation surgery is usually performed by a vascular or orthopedic surgeon. The diseased or severely injured part of the limb is removed, keeping as much of the healthy limb as possible. The surgeon shapes the remaining limb to allow the best use of a prosthetic leg after recovery.
The need for transtibial amputation is caused by conditions, including:
- Peripheral vascular disease (poor circulation).
- Diabetes.
- Infection.
- Foot ulcers.
- Trauma in which the lower leg is crushed or severed.
- Tumors (see link references at the bottom of the page for more information).
How Can a Physical Therapist Help?
Your physical therapist can help you prepare for below-knee amputation surgery. They also can help you regain strength, movement, and function after surgery.
Before Surgery
Before your surgery, your physical therapist may:
- Prescribe exercises for preop conditioning and to improve the strength and flexibility of your hip and knee.
- Teach you how to use a walker or crutches.
- Educate you and your family or caregivers about what to expect after the procedure.
Immediately After Surgery
Your hospital stay after surgery will be about five to 14 days. Your wound will be bandaged. You may also have a drain (a tube that is inserted into the area to help remove excess fluid). Your physician will help you manage your pain with proper medication.
Physical therapy will begin soon after surgery once your physician clears you for rehabilitation. A physical therapist will review your medical and surgical history and visit you at your bedside. Your first two to three days of treatment may include the following:
- Gentle stretching and range-of-motion exercises.
- Learning to roll in bed, sit on the side of the bed, and move safely to a chair.
- Learning how to position your leg to prevent contractures (the inability to straighten the knee joint fully). Contractures result from keeping the limb bent too much.
When you are medically stable, the physical therapist will help you learn to move about. They will teach you how to move using a wheelchair and stand and walk with an assistive device.

Rehabilitation
Your physical therapist will work with you as you heal and help to fit your prosthesis. They will guide your rehabilitation to help you regain your strength and movement in the safest way possible. Your treatments may include:
Prevention of contractures. A contracture is the development of soft-tissue tightness that limits joint motion. The condition occurs when muscles and soft tissues become stiff from lack of movement. The most common contracture after a below-knee amputation occurs at the knee. If the knee stays flexed (bent), you may be unable to straighten it. Using a pillow under your knee when resting in bed contributes to contractures. The hip also may become stiff.
It is essential to prevent contractures early. A contracture can become permanent if not addressed throughout recovery and after rehabilitation. Contractures can make it hard to wear your prosthesis. They also can make it difficult to walk and increase the need to use a walker or other assistive device.
Your physical therapist will help you maintain normal posture and range of motion at your knee and hip. They will teach you how to position your leg and show you stretching and other exercises to maintain a normal range of motion. Following your physical therapist's advice can help prevent a contracture.
Compression to reduce swelling. It is normal to experience swelling after surgery. Your physical therapist will help you maintain compression on your limb to protect it, reduce and control swelling, and help it heal. Compression can be accomplished by:
- Wrapping the limb with elastic bandages.
- Wearing an elastic shrinker sock.
These methods also help shape the limb to prepare it for fitting the prosthetic leg.
In some cases, a rigid dressing or plaster cast may be used instead of elastic bandages. An immediate postoperative prosthesis made with plaster or plastic also may be applied. The method chosen depends on each person's situation. Your physical therapist will help monitor the fit of these devices and instruct you in their use. The main goal of your care during this time is to reduce swelling.
Pain management. Your physical therapist will help you manage your pain in a variety of ways, including:
- Manual therapy, or "hands-on" treatments performed by your physical therapist. These may include soft tissue (muscle, tendon) mobilization, joint manipulation, or gentle range-of-motion exercises to improve circulation and joint motion.
- Residual limb management, including skin care and using a prosthetic shrinker.
- Desensitization to help address how sensitive an area is to clothing, pressure, or touch. This technique involves stroking the skin with distinct types of touch to help reduce or eliminate sensitivity.
- Mirror therapy or graded motor imagery to reduce phantom sensation or pain.
Around 80% of people who undergo amputations experience a phenomenon called phantom limb pain. It's a condition in which some pain feels like it is actually coming from the amputated limb. Your physical therapist will work with you to lessen and eliminate the sensation. See our Physical Therapy Guide to Phantom Limb Pain for more details.
Prosthetic fitting and training. Your physical therapist will work with a prosthetist to prescribe the best prosthesis for you. They will choose one designed for your mobility level, your life situation, and your activity goals. You will receive a temporary prosthesis at first. You will use it while your residual limb continues to heal, shrink, and shape over the first six to nine months after your amputation. The prosthesis will be modified to fit your leg as needed during this time.
Most people with transtibial amputations learn to walk well with a prosthesis. Physicians use the following criteria to determine when you are ready for a temporary prosthesis or your first artificial limb:
- Your incision should be almost healed or completely healed.
- Your swelling should have decreased to an acceptable amount.
- You will have regained sufficient overall strength to be able to walk safely.
After your limb has reached a stable shape and your physician approves your condition, you will be fitted for a permanent prosthesis.
Prosthetic and functional training. You will learn to function with more independence once you receive a prosthesis. Your physical therapist will help you master mobility tasks, daily activities, and walking with an assistive device. You will learn a daily skincare routine and how to check your limb for redness or blisters. It's also important to continue contracture prevention with exercise and positioning during this time.
Your physical therapist will teach you how to manage your new prosthesis. This might include learning to put it on and remove it and how to manage a good prosthetic socket fit. Your therapist will help you to gradually build up a tolerance for wearing your prosthesis. They will also teach you how to protect the skin of your residual limb. You may continue to use a wheelchair to get around even after you get your permanent prosthesis. Some people find it necessary to use a wheelchair for times when:
- Their limb is sore.
- They are having their prosthesis repaired.
- They are waiting on a new prosthesis.
Guided rehabilitation. Your physical therapist will help guide you throughout your recovery. Amputation rehabilitation is a long journey. It can take up to 1 to 1 ½ years to heal completely and return to normalcy, and you may experience some setbacks. Managing your limb and the new prosthesis will require practice to learn and master. Talk to your physical therapist about your goals for rehabilitation. Tell them about your family responsibilities, work activities, and favorite hobbies. This will help your therapist design a treatment plan to help you reach or exceed your goals. Rehabilitation is a team effort.
Return to Recreational and Sports Activities
If you are active or have a favorite sport, you may want to consult with a recreational physical therapist. Some physical therapists have a practice focusing on adaptive sports and helping people choose the right adaptive recreation equipment. See our article "Adaptive Sports: Staying Active While Living With a Disability" or our Health Center for People with Disabilities for tips and more information. The Amputee-Coalition has helpful information as well.
Depending on your personal goals and preferred activities, your physical therapist can help you return to sports such as golf, hiking, running, swimming, or cycling. A prosthetist can help you choose the best prosthetic device for taking part in these types of activities. You also may gain valuable advice from other people with amputations. Your physical therapist can help you find support groups in your area.
Can This Injury or Condition Be Prevented?
Over half of all vascular amputations may be preventable. The leading causes of transtibial amputation are related to PVD (poor circulation), complicated by diabetes. Diligent diabetes management and foot care can greatly reduce the risk of developing problems that lead to leg amputations.
Protect your feet by wearing shoes that fit correctly and maintain adequate space for your toes. Diabetic or orthopedic shoes are specially designed to protect your feet. It is also important to examine your legs and feet daily for signs of skin problems, such as a change in color, swelling, blisters, scratches, or open wounds. See our article "Feet First: Six Tips to Maintain Healthy Feet and the Freedom to Move" for more tips. Consult your health care provider right away if you notice a problem. Address problems early to prevent them from getting worse.
It is also important to stop smoking. Smoking cigarettes can greatly interfere with and delay wound healing in the feet and legs. Smokers with a prior amputation have a 25 times greater risk of reamputation (further removal) of the same limb than nonsmokers.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and training to treat people with amputations. However, you may want to consider a physical therapist who has experience treating people with lower limb amputations.
You can find physical therapists with these and other credentials in your area by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- Ask your physician or prosthetist if they work closely with a physical therapist.
- Ask about the physical therapists' experience in helping people with a below-knee amputation before making an appointment.
The American Physical Therapy Association believes that consumers should have access to information that could help them make health care decisions and prepare them for a visit with their health care provider.
The following articles provide some of the best scientific evidence related to physical therapy treatment of transtibial amputation. The articles report recent research and give an overview of the standards of practice for treatment of it both in the United States and internationally. The article titles are linked either to a PubMed* abstract of the article or to free full text, so that you can read it or print out a copy to bring with you to your health care provider.
US Department of Veterans Affairs website. VA/DoD clinical practice guidelines for rehabilitation of lower limb amputation. Published 2017. Accessed May 15, 2024.
Amputee Coalition Organization website. Accessed May 15, 2024.
Cancer Treatment Centers of America. Accessed May 15, 2024.
American Diabetes Association. Accessed May 15, 2024.
Digital Resource Foundation for the Orthotics & Prosthetics Community. Accessed May 15, 2024.
The O&P Edge. Accessed May 15, 2024.
Health.mil. Accessed May 15, 2024.
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine's MEDLINE database.
Expert Review:
May 15, 2024
Revised:
Jul 12, 2024
Content Type: Guide
Below-Knee Amputation
PT, board-certified clinical specialists in orthopaedic physical therapy
Chris Doerger
PT
Michael Verbsky
PT
Toran D. MacLeod
PT, MPT, PhD
Dawn Drumm
PT, DPT, on behalf of the Academy of Acute Care Physical Therapy
You Might Also Like...
Article
Wound Management in Physical TherapyJul 8, 2024
Physical therapists who are wound management specialists have additional skills and expertise to provide wound healing treatments. Learn more about wound
Health Tips
Feet First: 6 Tips to Maintain Healthy Feet and the Freedom to MoveJun 28, 2024
Feet are among the most important body parts. Learn how to take care of your feet with these foot care tips from physical therapists so you can keep moving
Video
Patient Story: Jun (From Amputee to Marathon Runner)Jul 22, 2019
Jun’s physical therapist helped him manage pain and achieve his movement goals after his left leg needed to be amputated below the knee to stop the spread


